Making the decision to bring home care into your loved one’s life is never easy. Most families wrestle with this choice for months, sometimes years. You wonder if you’re giving up too soon. You worry about what your parents or spouse will think. You question whether you’re doing enough on your own.
These feelings are normal. They’re also a sign that you care deeply about getting this right.
Dementia changes everything slowly, then all at once. One day your mom forgets where she put her keys. A few months later, she’s leaving the stove on. Before long, she doesn’t remember eating lunch or taking her medication. The person you’ve known your whole life starts to slip away in small moments that eventually add up to something you can’t ignore.
This article will help you understand when dementia home care stops being just an option and becomes the right choice for your family. We’ll walk through the signs that matter most, the safety concerns that keep you up at night, and the different types of support available. By the end, you’ll have a clearer picture of what your loved one actually needs and how to move forward with confidence.
Understanding the Progression of Dementia
Dementia isn’t one single disease. It’s an umbrella term for several conditions that affect memory, thinking, and the ability to handle daily tasks. Alzheimer’s disease is the most common type, but vascular dementia, Lewy body dementia, and frontotemporal dementia all fall under this category.
In the early stages, memory lapses seem like normal aging. Your dad might repeat the same story twice in one conversation. Your wife might struggle to find the right word for common objects. These moments are frustrating but manageable. Most people can still live independently with minimal help.
The middle stages bring bigger changes. Memory loss becomes more obvious and harder to work around. Your loved one might get lost in familiar places or forget the names of close family members. They might ask the same question ten times in an hour. Daily activities like cooking, managing finances, or taking medication correctly become difficult or dangerous without supervision.
Late stage dementia requires full time care. Communication becomes limited. Physical abilities decline. The person you’re caring for may not recognize you anymore. They need help with every aspect of personal care, from eating to using the bathroom.
Understanding where your loved one falls on this spectrum helps you plan ahead. It also helps you recognize that needing help isn’t a failure. It’s just the reality of how this disease works.
Why Timing Matters in Dementia Home Care
Many families wait too long to bring in outside help. This usually happens for understandable reasons. You don’t want to admit how bad things have gotten. Your loved one refuses to accept that they need assistance. You’re managing okay most days, so you convince yourself you can handle it a little longer.
But waiting too long creates real risks. Falls happen when no one is there to help with walking or balance. Medications get missed or taken twice. Wandering becomes more frequent and more dangerous. The stress on family caregivers builds until someone ends up in the emergency room, either the person with dementia or the exhausted family member trying to do everything alone.
Starting dementia home health care early gives everyone time to adjust. Your loved one gets used to having someone around while they can still build a relationship with their caregiver. You get the breathing room you need before you’re completely burned out. Safety measures get put in place before a serious accident happens.
Early intervention also slows the need for more intensive care later. When someone receives consistent support with daily routines, proper nutrition, and medication management, they often stay healthier and more functional for longer periods.
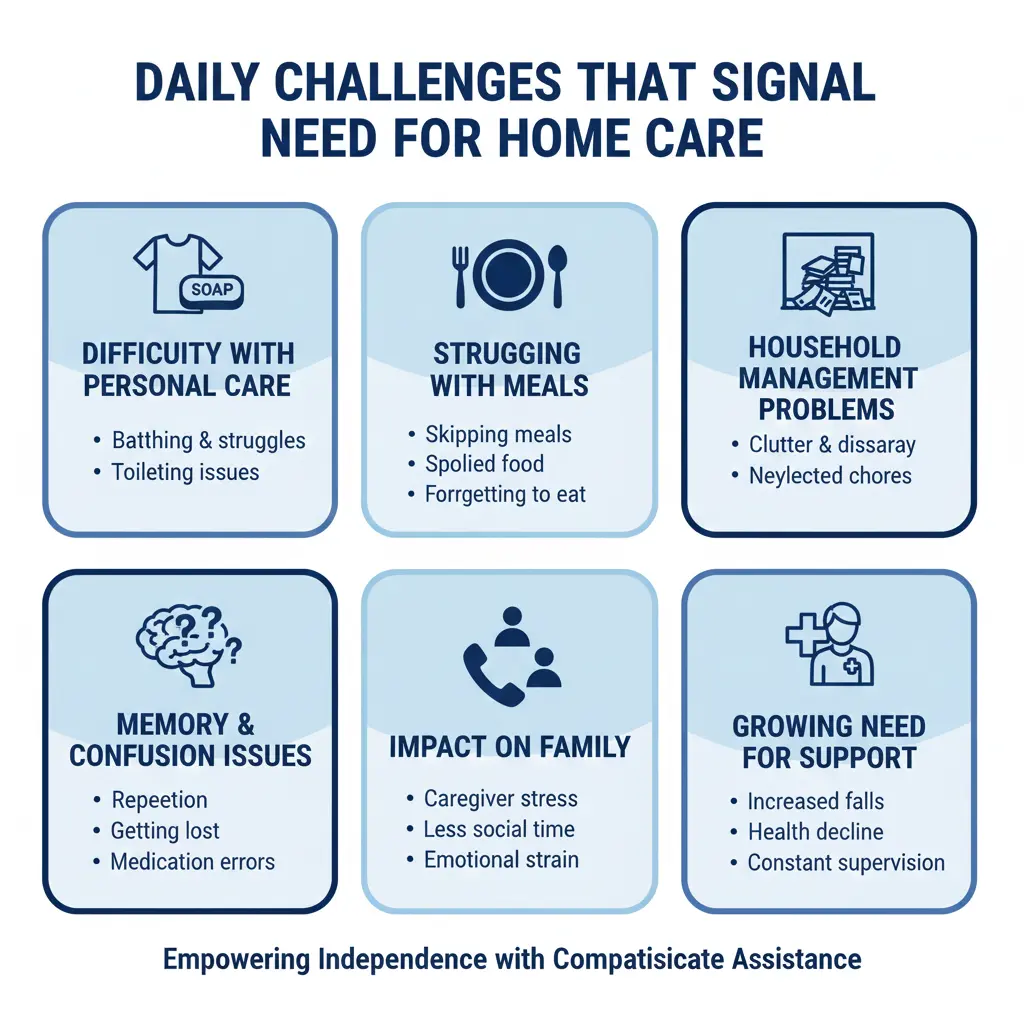
Daily Challenges That Signal the Need for Home Care
The decision to bring in help usually comes down to specific, recurring problems that you can’t solve on your own anymore. These aren’t dramatic crisis moments. They’re the daily struggles that pile up until you realize something has to change.
You notice your mom wearing the same clothes for days because getting dressed has become too confusing. Your husband stops showering regularly because he’s forgotten how or feels scared in the bathroom. Meals get skipped because cooking feels overwhelming or they simply forget to eat.
The mail piles up unopened. Bills don’t get paid. The house starts looking cluttered or dirty because your loved one can’t keep up with basic housekeeping anymore. These changes don’t mean they’re lazy or not trying. Their brain simply isn’t processing tasks the way it used to.
Phone calls at odd hours become more frequent. Your loved one is confused about what time it is or whether you already visited today. They might call multiple times about the same concern, forgetting they already talked to you. The constant worry about what might be happening when you’re not there starts affecting your own sleep and health.
These patterns tell you it’s time to consider bringing someone into the home on a regular basis. Not because you’ve failed, but because the disease has progressed to a point where professional support makes everyone’s life better and safer.

Memory Loss and Safety Concerns at Home
Memory loss creates safety hazards that most people don’t anticipate until something goes wrong. Your loved one might leave the front door unlocked or even wide open. They might let strangers into the house because they forget to be cautious. Car keys become dangerous when someone with dementia still believes they can drive safely.
Kitchen fires are more common than most families realize. Someone puts a pot on the stove and walks away, forgetting completely. The smoke alarm goes off, but they don’t remember what it means or how to respond. By the time you arrive, the situation could be life threatening.
Wandering happens with many types of dementia, especially Alzheimer’s. Your loved one might walk out of the house at night in their pajamas, convinced they need to go to work or find their childhood home. They can get lost within minutes, even in neighborhoods they’ve lived in for decades. Winter weather in Illinois makes wandering particularly dangerous.
Memory loss care at home il addresses these specific risks through consistent supervision and environmental modifications. Professional caregivers know how to redirect attention safely, create routines that reduce confusion, and spot warning signs before dangerous situations develop.
Medication management becomes critical as memory declines. Taking the wrong dose of heart medication or diabetes medication can send someone to the hospital quickly. Forgetting blood thinners or taking them twice both create serious medical risks. Having someone present to oversee medications removes this constant source of worry.
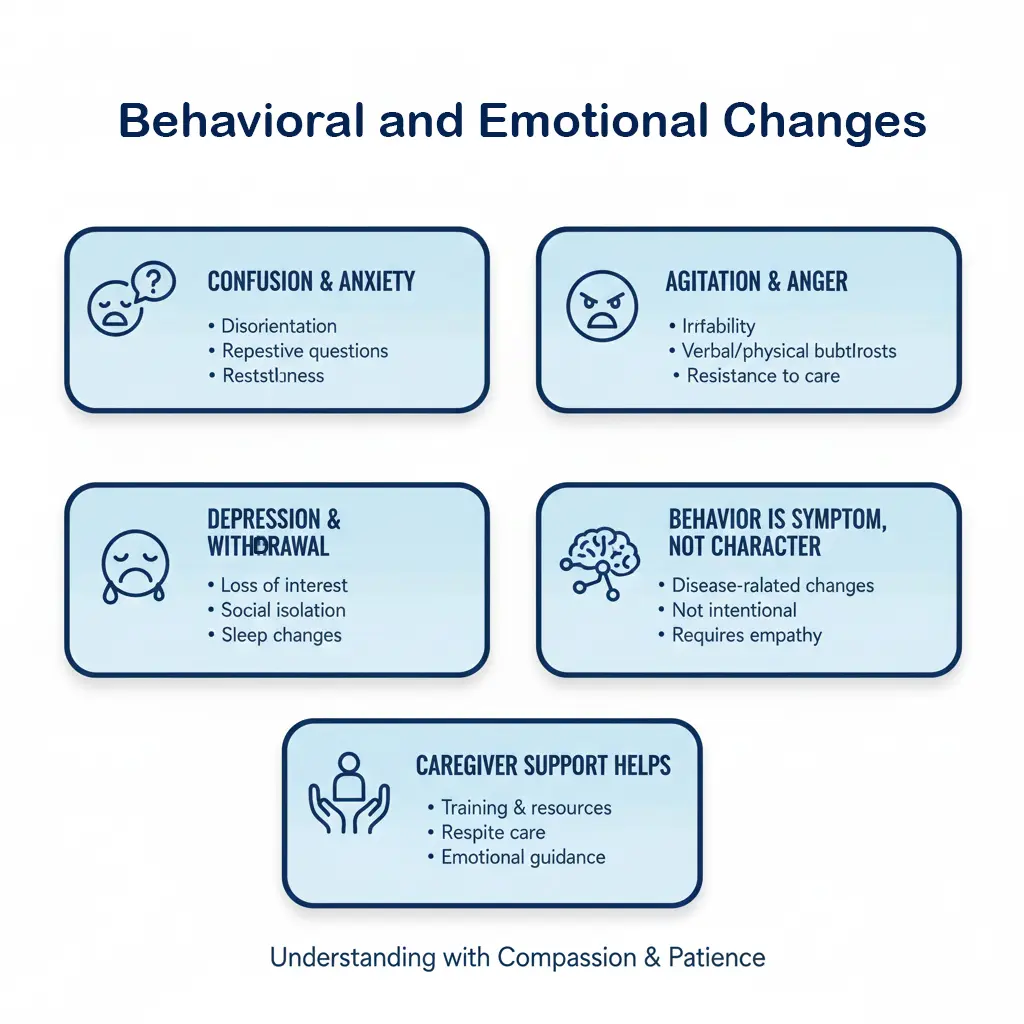
Behavioral and Emotional Changes
Dementia doesn’t just affect memory. It changes personality, emotions, and behavior in ways that can be heartbreaking and difficult to manage.
Confusion often leads to anxiety and fear. Your loved one might become convinced that someone is stealing from them or that strangers are in the house at night. These beliefs feel completely real to them, and logical explanations don’t help. The fear is genuine, even when the threat isn’t.
Agitation and anger can appear suddenly, especially later in the day. This is sometimes called sundowning. Your usually gentle mother might become irritable and accusatory as evening approaches. Your calm father might lash out verbally or even physically when he feels confused or scared.
Depression and withdrawal are common too. Some people with dementia lose interest in activities they used to love. They stop wanting to see friends or leave the house. The isolation makes everything worse, but they might resist all attempts to get them engaged with life again.
These behavioral changes are symptoms of brain damage, not character flaws. They’re also exhausting for family members who feel like they’re walking on eggshells all the time. Professional caregivers trained in dementia care know how to de-escalate difficult moments and provide emotional reassurance in ways that actually help.
Difficulty With Personal Care and Hygiene
As dementia progresses, basic self care becomes more challenging. This is often the hardest transition for families to navigate because it involves such intimate, personal tasks.
Bathing can become frightening for someone with dementia. The bathroom feels confusing. They might not remember what to do or feel afraid of falling in the shower. Resistance to bathing is extremely common and rarely about being stubborn. It’s usually about fear and confusion.
Getting dressed seems simple until it isn’t. Your loved one might put clothes on in the wrong order or refuse to change out of dirty clothes. They might dress inappropriately for the weather, wanting to wear winter coats in July or shorts in January. The simple act of choosing an outfit and putting it on correctly requires multiple steps that become overwhelming.
Eating and drinking enough becomes an issue when people forget meals or lose interest in food. Some people with dementia develop strange food preferences or want to eat the same thing every day. Others stop being able to use utensils properly or forget how to chew and swallow safely.
Toileting and incontinence are among the most difficult challenges for family caregivers. Your loved one might forget where the bathroom is or not make it there in time. They might need reminders to use the toilet regularly. Eventually, they may need help with all aspects of personal hygiene.
Many adult children struggle with providing this level of intimate care for their parents. The role reversal feels wrong. Your parents may also resist accepting this kind of help from you specifically. Professional caregivers can often provide personal care more easily because they’re trained for it and there’s no complicated emotional history involved.
The Role of Companion Care for Dementia Patients at Home
Not every situation requires hands on physical care right away. Sometimes what your loved one needs most is companionship, supervision, and help staying engaged with daily life.
Companion care for dementia patients at home focuses on providing consistent presence and emotional support. A caregiver might spend time talking, looking at old photos, or helping with hobbies and activities your loved one still enjoys. Even when conversation becomes limited, having someone there reduces anxiety and loneliness.
Supervision is a major component of companion care. The caregiver makes sure your loved one stays safe while you’re at work or running errands. They redirect harmful behaviors gently. They keep routines consistent, which helps reduce confusion. They notice changes in condition early and can alert family members before small problems become emergencies.
Meal preparation and light housekeeping often fall under companion care as well. Having someone there to prepare lunch and ensure it gets eaten solves multiple problems at once. A caregiver can also help with laundry, tidying up, and other tasks that keep the home environment safe and comfortable.
Social interaction matters enormously for people with dementia. Regular visits from the same caregiver provide structure and relationship. Many people with memory loss respond well to having a consistent routine with a familiar face. They may not always remember the caregiver’s name, but they remember the feeling of being cared for.
Companion care works particularly well in the early to middle stages of dementia. It provides the support your loved one needs while allowing them to maintain as much independence as possible. It also gives family caregivers reliable breaks without the guilt of leaving their loved one alone.
When a Personal Care Aide Becomes Necessary
As dementia advances, companion care isn’t enough anymore. Your loved one needs someone who can provide hands on assistance with bathing, dressing, grooming, and other intimate care tasks.
Personal care aides are trained to help with activities of daily living in a way that preserves dignity. They understand how to approach someone who’s resistant to bathing or dressing. They know safe transfer techniques for someone who’s unsteady on their feet. They can handle incontinence care with professionalism and compassion.
The transition to needing this level of care is difficult for everyone involved. Your loved one may feel embarrassed or angry about losing independence. Family members often feel guilty about bringing in outside help for such personal tasks. These feelings are valid and normal.
Personal care aide dementia patients lemont il services can be scheduled for specific times of day when help is most needed. Some families bring in an aide for morning care to help with showering and dressing. Others need evening assistance with dinner and bedtime routines. The schedule adapts to your family’s specific situation.
Having professional help with personal care often improves the relationship between family caregivers and their loved one. When you’re not constantly battling over bathing or changing clothes, you can spend your time together doing things you both enjoy. The caregiver role becomes less about wrestling with difficult tasks and more about preserving connection and quality of life.
Caregiver Burnout and the Need for Respite
Family caregivers often push themselves far beyond reasonable limits. You miss work to handle appointments. You lose sleep listening for sounds in the night. Your own health starts to suffer because you’re not eating right, exercising, or seeing your doctor. Relationships with your spouse or children become strained because dementia care takes up all your time and energy.
This isn’t sustainable. Caregiver burnout is a real medical concern with serious consequences. Studies show that family caregivers of people with dementia have higher rates of depression, anxiety, and physical health problems. Some caregivers die before the person they’re caring for because the stress literally shortens their life.
Respite care gives family caregivers essential breaks. This isn’t about shirking responsibility or being selfish. It’s about recognizing that you can’t pour from an empty cup. Taking time to recharge makes you a better caregiver when you return.
Respite care for dementia patients lemont il can be scheduled for a few hours a week or for longer periods when you need time away. Maybe you have your own medical procedures to handle. Maybe you need to visit family out of state. Maybe you just need a weekend to sleep and remember what it feels like to not be in crisis mode.
Some families resist respite care because they feel guilty leaving their loved one with a stranger. But regular respite care actually benefits the person with dementia too. They get socialization with someone new. Family relationships improve when you’re not exhausted and resentful. Everyone’s quality of life goes up.
The key is starting respite care before you’re at the breaking point. If you wait until you’re completely burned out, you’re already in crisis mode. Early, regular breaks prevent that crisis from happening.
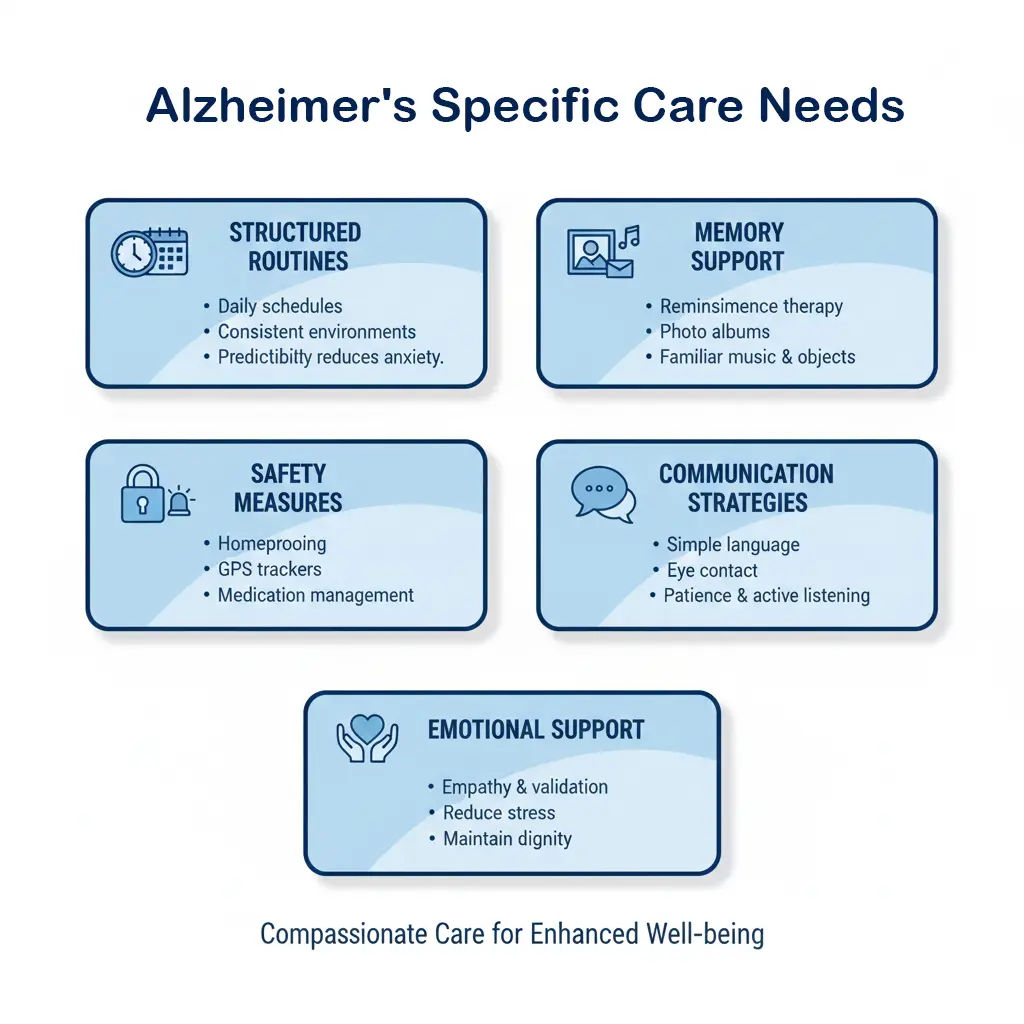
Alzheimer’s Specific Care Needs
Alzheimer’s disease has some unique characteristics that require specific care approaches. While it shares many symptoms with other types of dementia, the progression and challenges can look different.
People with Alzheimer’s typically benefit from highly structured routines. The same activities at the same time each day reduce confusion and anxiety. When everything is predictable, the world feels safer and more manageable.
Alzheimer’s home care Illinois often incorporates memory enhancing activities and environmental modifications. Caregivers might use music, photos, and familiar objects to help ground someone in the present moment. They create memory boxes with meaningful items that can spark recognition and conversation.
Safety becomes increasingly important as Alzheimer’s progresses. Wandering is particularly common with this type of dementia. Door alarms, secure locks, and vigilant supervision help prevent dangerous situations. Some caregivers use identification bracelets or tracking devices for added security.
Communication changes with Alzheimer’s in predictable patterns. Your loved one might lose nouns first, then struggle with more complex language. Eventually, verbal communication becomes very limited. Caregivers trained in Alzheimer’s care know how to communicate through tone of voice, body language, and simple, clear language.
The emotional experience of Alzheimer’s is important to understand. Even when your loved one can’t express it clearly, they often sense that something is wrong. They may feel frustrated, scared, or sad about their declining abilities. Compassionate care acknowledges these feelings and provides comfort without trying to fix what can’t be fixed.
In-Home Memory Care vs Other Care Options
When dementia care becomes necessary, families face several options. Understanding the differences helps you make the choice that fits your specific situation.
In home memory care Illinois allows your loved one to stay in familiar surroundings. This often reduces confusion and anxiety because they’re in their own space with their own belongings. Routines can stay more consistent. Pets remain part of daily life. The person with dementia doesn’t have to adjust to a new environment, which can be very disorienting.
Home care is flexible. You can start with just a few hours a week and increase gradually as needs change. You can schedule care for specific times of day when help is most needed. Multiple family members can still be involved in caregiving while professional help fills the gaps.
Adult day programs provide structured activities and socialization during daytime hours. Your loved one spends the day at a facility with others who have similar conditions, then returns home in the evening. This works well for people who are still fairly social and benefit from stimulation, while giving family caregivers daytime hours for work or rest.
Assisted living memory care units offer 24hour supervision in a residential setting. This becomes necessary when round the clock care is needed and providing that at home is no longer feasible. Memory care facilities are designed specifically for people with dementia, with secure environments and trained staff.
Nursing homes provide the highest level of medical care. This option makes sense when someone has complex medical needs beyond what can be managed at home or in assisted living. Late stage dementia often requires this level of care.
Many families use a combination of these options over time. You might start with home care, add adult day services as social needs increase, and eventually transition to residential care when 24hour supervision becomes necessary. There’s no one right path. The best choice is whatever works for your family right now, with flexibility to change as needs evolve.
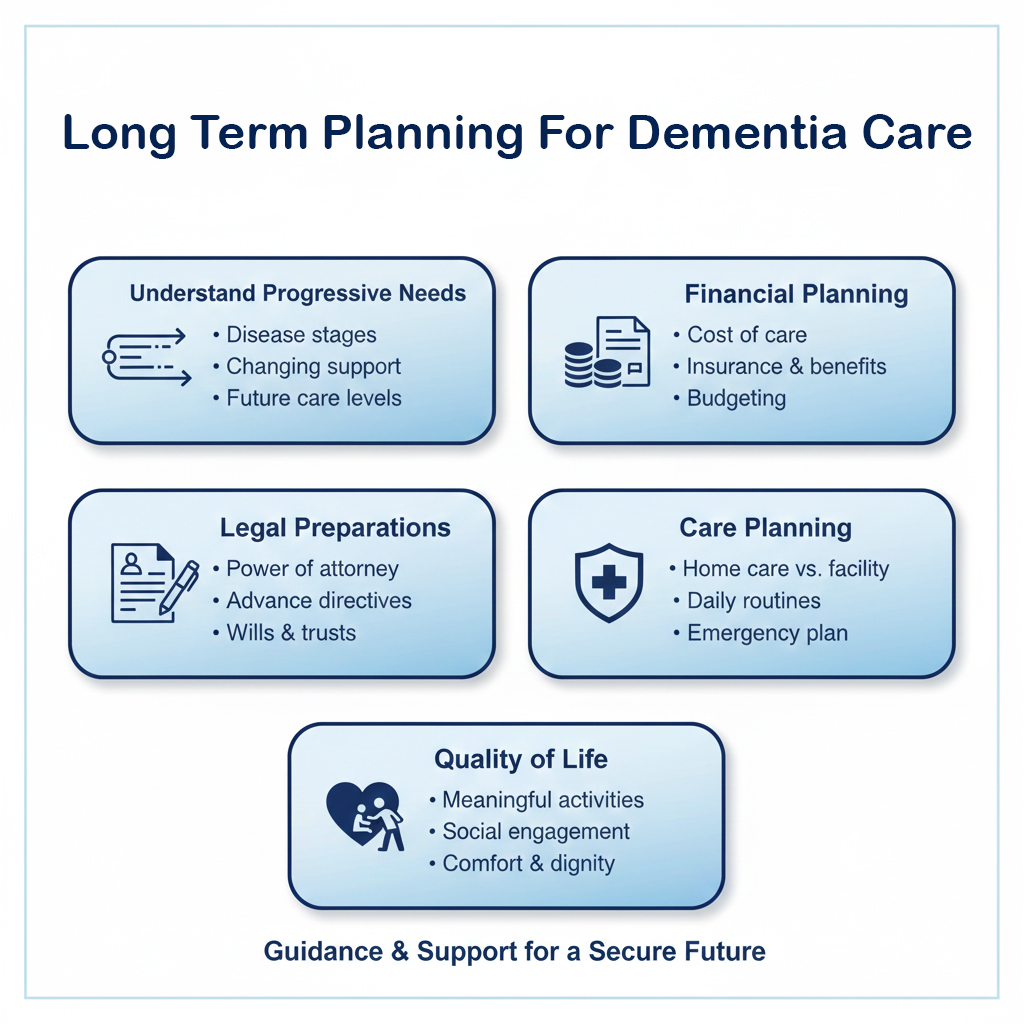
Long Term Planning for Dementia Care
Dementia is a progressive condition. Planning ahead helps you make better decisions and reduces crisis situations down the road.
Long term care services dementia illinois includes multiple types of support that might become necessary over time. Understanding what’s available and how to access these services makes the journey less overwhelming.
Financial planning is crucial. Dementia care is expensive, whether provided at home or in a facility. Medicare covers some medical costs but not custodial care. Medicaid has income and asset requirements that take time to navigate. Long term care insurance, if your loved one has it, has specific rules about when and how benefits can be used.
Many families wait too long to explore financial options. Starting these conversations early, ideally when your loved one can still participate in decisions, makes everything easier. An elder law attorney can help you understand legal and financial strategies that protect assets while ensuring quality care.
Legal documents need attention early in the disease process. Power of attorney for healthcare and finances should be established while your loved one can still legally sign documents. Advanced directives clarify wishes about medical treatment. These documents prevent family conflict and legal complications later.
Care planning involves thinking through scenarios you hope won’t happen but might. What if the primary family caregiver gets sick or injured? What if your loved one’s condition declines faster than expected? Who will make decisions if family members disagree? Having these conversations before a crisis hits leads to better outcomes.
Support for the person with dementia includes planning for quality of life, not just safety. What activities still bring joy? What relationships matter most? How can you preserve dignity and personhood as abilities decline? These questions matter just as much as logistics and finances.
Valentine Home Health Care
Valentine Home Health Care provides dementia care services throughout Illinois with a focus on keeping people safe and comfortable in their own homes. Their caregivers receive specialized training in memory loss care and understand the unique challenges that come with Alzheimer’s and related conditions. The agency works with families to create care plans that address specific needs, whether that involves medication reminders, meal preparation, personal care assistance, or full time supervision. They offer both short term respite care and long term care coordination, adjusting services as conditions change over time. Valentine emphasizes building consistent relationships between caregivers and clients, recognizing that familiarity and routine help reduce anxiety for people with dementia.
How Families Can Decide When the Time Is Right
There’s no perfect moment when you suddenly know for sure it’s time to bring in help. Instead, you look at patterns and trends. You pay attention to what’s not working anymore.
Ask yourself honest questions. Is your loved one safe when alone? Are medications being taken correctly? Is nutrition adequate? Are basic hygiene needs being met? If the answer to any of these is no, it’s time.
Consider your own wellbeing too. Are you sleeping? Can you maintain your job? Are your other relationships suffering? Do you snap at your loved one more often than you’d like? These signs matter because sustainable care requires healthy caregivers.
Talk with your loved one if possible. Some people with early stage dementia can participate in care planning. They might even feel relieved to know help is coming. Others will resist strongly. You may need to introduce caregivers gradually, perhaps framing it as help for you rather than help for them.
Involve other family members in the decision. Different perspectives help you see the full picture. Someone who visits occasionally might notice changes you’ve been too close to see. Just make sure these conversations happen with compassion for everyone involved, including the person with dementia.
Trust your instincts. If you’re constantly worried, that worry is telling you something. If you’re waking up at 3 AM mentally running through worst case scenarios, your gut already knows the situation needs to change.
Start small if you’re not ready for full time care. Bring someone in for a few hours twice a week. See how it goes. Most people find that once help is in place, they wish they’d done it sooner.
Common Questions Families Ask
How much does dementia home care cost?
Costs vary based on how many hours of care you need and what level of care is required. Companion care costs less than skilled nursing care. Most agencies charge by the hour, with discounts for longer shifts or full time care. Your specific location in Illinois also affects pricing.
Will my loved one accept help from a stranger?
Maybe not at first. Resistance is common and normal. Many people with dementia adapt better than families expect once a routine is established. The key is finding the right caregiver match and giving the relationship time to develop.
Can I choose who provides care?
Most home care agencies try to accommodate preferences. You can request specific traits in a caregiver, like someone who speaks a particular language or shares interests with your loved one. Building consistency with one or two regular caregivers helps tremendously.
What if my loved one’s condition gets worse?
Good home care agencies adjust services as needs change. You can increase hours, add different types of care, or transition to 24hour supervision. The flexibility is one of the main benefits of home care over residential placement.
How do I pay for long term care?
Options include private pay, long term care insurance, veterans benefits, and eventually Medicaid for those who qualify. Each funding source has different rules and requirements. A consultation with an elder care financial planner can clarify your specific options.
Is home care better than a memory care facility?
Neither is universally better. Home care works well when someone can still benefit from familiar surroundings and family involvement. Residential memory care becomes necessary when 24hour supervision is required or when the home environment can’t be made safe enough. Many families use home care for as long as possible, then transition to residential care when needs exceed what can be provided at home.
Conclusion
Deciding when dementia home care becomes necessary is one of the hardest choices you’ll face as a family caregiver. There’s no single right answer that works for everyone. But there are signs you can watch for, questions you can ask yourself, and support available when you’re ready to reach for it.
Your loved one deserves to be safe, comfortable, and treated with dignity. You deserve to maintain your own health and wellbeing while providing care. These things aren’t in conflict. Professional home care makes both possible.
The decision to bring in help isn’t about giving up or admitting defeat. It’s about recognizing that dementia is a disease that eventually requires more support than one person or even one family can provide alone. Accepting that reality takes courage.
Trust yourself. You know your loved one better than anyone. You see what’s happening day to day. When you feel that pull toward getting help, listen to it. Starting care services earlier rather than later almost always leads to better outcomes for everyone involved.
You’re not alone in this journey. Thousands of families across Illinois are navigating the same challenges. Resources exist to help you, whether you’re just starting to notice changes or you’re deep into caregiving and need relief. Taking the first step toward getting support might feel overwhelming, but you’ll likely look back and realize it was the moment things started to get a little bit easier.
Your loved one’s story matters. So does yours. Getting the right support in place helps you both move forward with more safety, less stress, and the ability to hold onto the moments of connection that still remain. Read more







